Why Do People Have a Blind Spot in Vision? Scotoma Explained
Have you ever experienced a sudden gray spot in vision? Or maybe you’ve heard about these things called scotomas? They’re like temporary blind spots in vision that can show up in your eyes. It’s like a little mystery in the world of eyesight that both eye experts and ordinary people find interesting. Imagine seeing something gray or a bit fuzzy in one part of your vision, making it tricky to see clearly for a little while. That’s what a scotoma is like. It can come and go or sometimes stay longer. Let’s dive into the curious world of scotomas, where we’ll unravel the secrets behind these temporary blind spots.
Blind Spots in Vision – What is a scotoma
A scotoma refers to a sudden blind spot in vision, and its duration—whether temporary or permanent—depends on the underlying cause. Some terms, like “scotomata,” are used interchangeably for multiple scotomas. While many cases result in a permanent condition, leading to a significant decline in optimal functioning, scotoma is not a standalone disease. Instead, it is a symptom indicative of an underlying disorder or condition.
Manifesting as a blurry or blind spot in the eye, scotoma can appear in various locations and configurations. Whether unilateral or bilateral, singular or multiple, scotomas warrant professional attention for addressing the root cause and exploring appropriate treatment options. Seeking prompt medical assistance is recommended for individuals experiencing scotomas to manage the underlying conditions effectively.
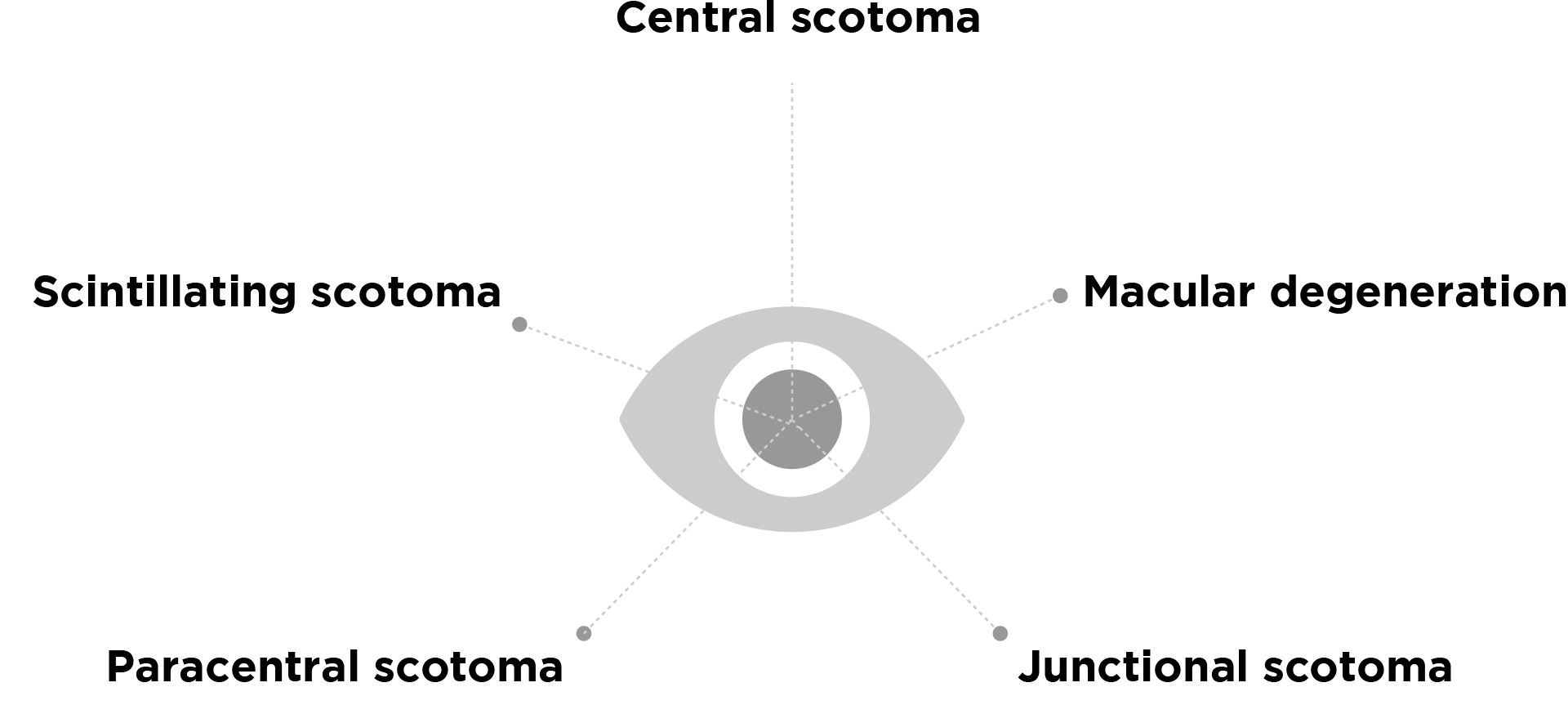
Types of Scotomas
There are various types of scotoma in the eye, each characterized by distinct features and manifestations. The classification of these types often depends on the location of the blind spot and may even incorporate colors.
Scotomas can be categorized as positive or negative. In positive scotomas, individuals perceive something, like a spot of a specific color, whereas negative scotomas go unnoticed by the person, typically requiring identification during testing by healthcare providers. These terms also distinguish between occurrences in one eye (unilateral or monocular) and both eyes (bilateral or binocular).
Scotoma Examples:
- Central scotoma: A central scotoma refers to a blind spot situated directly in the center of your vision, aligning with your line of sight. These scotomas are particularly impactful as they can severely hinder activities like reading, driving, and recognizing faces, rendering them challenging or impossible.
- Macular degeneration, diabetic retinopathy, or diabetic macular edema are common causes of central scotomas. Additionally, eye infections and injuries affecting the macula of the retina can contribute to the development of a central scotoma.
- Scintillating scotoma: A scintillating scotoma is a visual disturbance typically observed in the paracentral or mid-peripheral region of the visual field. Interestingly, this type of scotoma may exhibit movement across the field of view rather than being confined to a single spot. Characterized by a more visual disturbance quality, with “scintillating” meaning “sparkling” or “shimmering,” it is often referred to as a visual aura. Typically associated with migraine headaches, it can occur independently without head pain. These scotomas are transient, lasting from a few seconds to up to 30 minutes, featuring arc- or ring-shaped patterns with wavy or jagged borders. Additionally, they may display a range of colors or alternate between light and dark shades of gray.
- Paracentral scotoma: A paracentral scotoma refers to a blind or blurry spot in your vision that lies slightly off-center, typically within 10 degrees of your line of sight. For instance, if you possess a paracentral scotoma and focus on a road sign, you might clearly see the words on the sign, but an adjacent area or spot very near the sign could appear dark or blurry. Conditions such as glaucoma and diabetic retinopathy are known to cause paracentral scotomas. In instances of glaucoma, the scotoma may take on an arc-shaped form, earning the designation of an arcuate scotoma. It’s possible for a paracentral scotoma to manifest on its own, or there may be multiple blind spots in your vision. In certain scenarios, a paracentral scotoma or multiple scotomas may coincide with peripheral vision loss, resulting in the commonly termed “tunnel vision.”
- Junctional scotoma: Caused by damage at the intersection of the optic nerve and optic chiasm, junctional scotomas result from impairments near the base of the brain where the optic nerve enters.
Scotoma Causes
Scotomas can arise from various causes, including:
- Eye injury
- Retinitis pigmentosa
- Glaucoma
- Trauma to the head
- Allergic reactions
- Stroke
- Diabetic retinopathy
- Hypertension and hypotension
- Sclerotherapy
- Macular degeneration
Scotoma Symptoms
Symptoms of scotomas vary based on their location within your visual fields. Central scotomas, situated in the central vision, pose significant challenges for daily activities. Recognizing faces, reading regular-sized prints, and discerning color and detail become difficult. Tasks like driving and using computers may be challenging, but peripheral vision works better when looking to the side and in dim light.
Peripheral scotomas have a milder impact unless they’re extensive, hindering side vision and potentially causing collisions when walking. Vision tends to perform better in bright light conditions.
Scintillating scotomas, often associated with migraines, manifest as shimmering bright areas preceding headaches. Starting as a small shimmer, they expand to cover half the visual field with bright spots and colorful rays. Vision typically recovers in about 15 minutes, followed by an intense migraine headache.
Scintillating scotomas can also result from conditions like high blood pressure, optic nerve inflammation, multiple sclerosis, and head injuries.
Risk Factors for Scotomas
Various factors may elevate the risk of developing scotomas in certain individuals.
Genetic predisposition to retinitis pigmentosa, glaucoma, diabetes, and obesity increases the likelihood of scotomas. Other general risk factors for scotomas include Hypotension, Migraine, Raynaud’s phenomenon (skin color changes in response to stress or cold), Snoring, Frequency of disc hemorrhage.
Notably, a study found that lifestyle factors like smoking did not significantly contribute to the risk of experiencing a scotoma.

How Scotomas Are Diagnosed
The detection of visual aura involves various diagnostic methods, primarily visual field tests and dilated eye exams.
Visual Field Tests
Commonly referred to as a Humphrey visual field test, this evaluation entails gazing into a bowl-shaped device. Administered by an eye care specialist, the test generates a detailed visual field map of the eyes, offering insights into the presence and extent of any scotomas.
Dilated Eye Exams
As part of the automated visual field test, pupils may be dilated using specialized eye drops. Subsequently, the eye specialist conducts a thorough examination of the eye, focusing on the optic nerve and retina. This comprehensive assessment aids in identifying the nature and characteristics of the scotoma.
Finding a blind spot in eye by yourself
Discovering your blind spot can be done with a simple pen-and-paper test or by using your hands. Here’s how:
Pen-and-Paper Test:
- Draw a small dot on one side of a wide piece of paper.
- Create a small plus (+) sign six to eight inches to the right of the dot.
- Close your right eye and hold the paper about 20 inches from your face.
- Focus on the plus sign while gradually bringing the paper closer.
- When the dot disappears, you’ve identified the blind spot in your left eye.
To find the blind spot in your right eye:
- Close your left eye and focus on the dot.
- Move the paper until the plus sign disappears.
Hand Test:
- Close your left eye and extend your left thumb at arm’s length.
- With your right eye, focus on your left thumb.
- Extend your right thumb next to the left thumb.
- While keeping your eye on the left thumb, slowly move the right thumb to the right.
- Your right thumb will seem to disappear when it reaches your blind spot.
To find the blind spot in your left eye:
- Close your right eye and gaze at your right thumb while moving the left.
Treatment for Scotomas
The approach to treating scotomas hinges on the underlying cause and type of visual impairment.
- Scotomas linked to migraine headaches are usually transient, resolving within approximately 30 minutes without specific treatment.
- If high blood pressure, stress, or other identifiable conditions contribute to scotoma development, addressing these factors through medications or other treatments may help prevent future occurrences of blind or blurry spots in your vision.
- Unfortunately, many scotomas resulting from conditions such as glaucoma, diabetes, macular degeneration, and specific neurological disorders lack definitive treatment options. However, in such cases, your eye doctor might recommend specialized low vision aids to assist you in managing vision loss related to scotomas, enabling you to utilize your remaining vision more effectively.
In conclusion, understanding the phenomenon of scotomas opens a fascinating window into the complexities of our vision. Everyone possesses a blind spot in their eye, situated where the optic nerve meets the retina, commonly known as a scotoma. Despite its constant presence, the majority of individuals are oblivious to their usual blind spot. Certain scotomas might indicate a serious eye issue such as glaucoma or macular degeneration. If you detect a blind spot or encounter visual disruptions affecting your everyday activities, it’s advisable to consult an eye doctor promptly.
Temporary scotomas are often triggered by brain disorders like seizures, migraines, or reduced blood flow. Fixed, permanent blind spots can be a result of disorders affecting the optic nerve, such as in glaucoma (increased eye pressure) or multiple sclerosis. Brain-related causes, like tumors or strokes, can also lead to permanent blind spots.
They are typically not permanent but may indicate an underlying health issue. Scotomas, which are auras or blind spots affecting part of your vision, can appear temporarily. Scintillating scotomas, like other types, may manifest as floaters, dots, or blind spots in your visual field.
In addition to migraines, scintillating scotomas can be influenced by factors such as stress, hormonal changes, and hypertension or high blood pressure.